Democratizing Access to Value in Healthcare: A Conversation with Pearl Health’s Chief Product Officer Jennifer Rabiner
All Posts Conference 2022 Direct Contracting Provider Tech Value Based Care
Pearl Health is a start-up on a mission to democratize access to value in healthcare. Pearl empowers primary care physicians to deliver better quality care for their patients at a lower cost via a physician enablement technology platform and a value-based payment model. Pearl’s technology provides simple financial reporting, visibility into patient panel health, and recommendations to allocate time and resources to deliver care to patients who need it most. Financially, Pearl helps primary care physicians transition from unpredictable, volume-based fee-for-service billing and reimbursement to stable per-patient-per-month payments, coupled with the opportunity to generate shared savings by enabling physicians to bear and capture value from risk-based payment models.
In September 2021, Pearl Health announced a $18M Series A funding led by Andreessen Horowitz, with follow-on funding from AlleyCorp, who invested in its seed round. Pulse Writer Lauren Gardanier sat down with Chief Product Officer, Jennifer Rabiner, to discuss CMS’ new Direct Contracting model and Pearl’s vision for better primary care under this new payment model.

Jennifer Rabiner, Chief Product Officer at Pearl Health
The Pulse: In your career, you’ve worked in a variety of healthcare settings – consulting, pharma, healthcare technology. What insights have you gained from those experiences and how do you draw on those experiences in your current role at Pearl Health?
Rabiner: The common threads across my career have been reimbursement and access to healthcare. For the first 10 years at Triage Consulting and Deloitte Consulting, I focused on the healthcare revenue cycle — how providers charge, bill and collect for services provided — and how to apply technology to optimize these processes. In my role at Millennium Pharmaceuticals, I again focused on reimbursement, working to remove provider, patient, or payer barriers to ensure reimbursement for the oncology drug we sold. These first chapters in my career were excellent lessons in the complexity and challenges inherent in how we pay for healthcare.
athenahealth was a very pivotal time in my career, during which I focused on building population health and value-based care technology in some of the earlier years of the shift from volume-based to value-based reimbursement. It was during this time that I started to see how important it is to change the underlying payment models for healthcare if we want to see a true transformation. More specifically, I realized that we can’t continue to do small improvements and iterations and see the kind of progress we know we need to make in order to reach the end-goal of better quality care at a lower cost with greater patient and provider satisfaction.
My next role at Hint Health supported doctors in the Direct Primary Care (DPC) model, under which doctors don’t do traditional billing. They earn revenue in the form of stable monthly payments for each of their patients, almost like a subscription, paid directly from a patient or employer. It’s truly a different model of care that is unencumbered by the predominant (and problematic) payment model in healthcare, known as fee-for-service (FFS). The FFS model is problematic because it incentivizes delivering a high volume of care rather than high value care, is administratively cumbersome, and indirectly creates a narrow care model since most activities that are reimbursable have to happen during a visit. In DPC, doctors have so much more flexibility in terms of how they care for their patients so that it can be tailored to the patient and the need. I learned a lot about what is possible in healthcare from the DPC community, and was really inspired by that world.
In many ways, Pearl Health is a natural culmination of these last two chapters. We support primary care providers in taking on value-based risk, which involves many of the same components as my focus at athenahealth with one big difference – we are also evolving the underlying payment model for primary care doctors and shifting a portion of their revenue to a per-member-per-month payment. This type of revenue model opens up so many doors for how providers can care for their patients, which means that we can start employing some of the same strategies that DPC doctors have already been successful in implementing.
The Pulse: What is CMS’ new Direct Contracting model? How will it impact the way care is provided to patients?
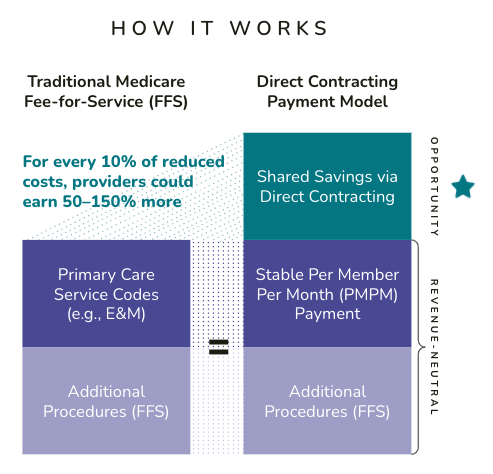
Rabiner: Large scale VBC programs, like Direct Contracting, seek to shift physician incentives to deliver high value care instead of high volumes of care. The government is trying to bend the cost curve, while ensuring high levels of clinical quality and patient satisfaction.
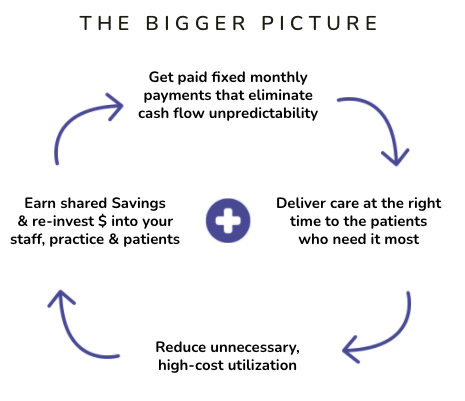
One key component of the program is the opportunity for a Direct Contracting Entity (DCE) to earn shared savings. In this model, a financial benchmark is calculated for each patient panel. If providers spend less than the benchmark, Medicare will share the savings with the Direct Contracting Entities (DCEs), which in turn share the savings with their providers. If the total cost of care exceeds the benchmark, Medicare will share these losses with DCEs, which may also share in these losses with their providers (if the provider has agreed to this type of arrangement). For many providers, this is exciting because it’s an opportunity for them to capture the full dollar value generated from effectively managing care for their Medicare patients, and they can use these funds to reinvest in their staff, their practices, and their patients.
Quality management is another component of Direct Contracting. In the standard Direct Contracting model, there are three clinical quality measures and a set of patient satisfaction measures that are tracked and factor into the final amount of shared savings a DCE can achieve.
One of the key differences in Direct Contracting over prior CMS models is the move to a capitation model for primary care reimbursement, the fixed per-member-per-month fee that I mentioned earlier. This fee gets paid in lieu of traditional fee-for-service reimbursement for the majority of primary care services. Under capitation, reimbursement is no longer tied to billable visits completed by billable providers. Instead, physician practices have more flexibility to deliver care in the way that is right for the patient, whether that’s an office visit longer than the standard 15 minutes, a virtual visit with a Medical Assistant, asynchronous communication with the office, or even a home visit.
In terms of how Direct Contracting will impact patient care, our goal is that patients whose physicians are enrolled in the model will actually start getting more tailored care specific to their needs due to the additional flexibility their physicians have in a capitation model. Direct Contracting applies to the Traditional Medicare population, and these patients retain all the
same rights and benefits they have in Medicare; there is no limiting of choice or extra fees. Doctors make the choice to participate in the Direct Contracting model, and their patients experience the benefits of value-based primary care.
The Pulse: What is Pearl’s mission and how are you enabling Direct Contracting participation to help achieve it?
Rabiner: Pearl’s mission is to democratize access to value in healthcare. Primary care plays a pivotal role in directing care for patients. We are empowering doctors to find opportunities for themselves, starting with Direct Contracting, and succeed in those opportunities. With the capitation model, we have real opportunity to build new workflows and care models to create a more
continuous and longitudinal approach to patient care. But this isn’t about becoming an EMR; this is about expanding the definition of caring for and managing a patient. Pearl is focusing on physician practice enablement to create new opportunities that aren’t anchored on a billable visit.
The Pulse: Could you share more about what Pearl’s engagement with providers for new workflows and care models might look like?
Rabiner: The initial workflows that we are rolling out are focused on two key areas: first, identifying and engaging with high-needs patients who have not been seen by the practice for an extended period of time. This patient engagement could be a visit, or it could be a call, email, or text – we want to redefine patient engagement to expand beyond a traditional visit. The underlying goal here is to help providers start taking a panel management approach, providing visibility into what’s happening with all of their patients, not just the ones who are coming in.
Second, we are building workflows related to patient admissions and discharges, from either ED or an inpatient setting. The three standard [Direct Contracting] quality measures are related to admissions, readmissions, and following up after hospital discharges. With this type of workflow, we want to be able to not only inform a practice that a patient is in the hospital, but once the patient is discharged, ensure the right interactions or visits happen so patients follow discharge plans and avoid being readmitted.
We are also really prioritizing the user experience as we build out these workflows. We want the people using our product to feel productive and encouraged by their progress. So much of the existing healthcare tech out there is so focused on doing a job, and doesn’t really consider how the human using the product is interacting with it.
The Pulse: Pearl Health is currently working with the Medicare population – as you look ahead, do you expect to expand beyond Medicare? What do you think are the challenges or opportunities of expanding to broader patient populations?
Rabiner: Direct Contracting is our initial go-to-market focus. We want to build this technology-enabled care model to manage patients, and Direct Contracting gives us a great path to accelerate this work. Once we have the technology and workflows, our next opportunity will be to sync up with other payers that want to support this world, similar to what CMS is doing right now. The best thing I could hear in a year is ‘I want to use Pearl for all my patients’. CMS and Direct Contracting will be our launching ground to learn how to do all of this, but certainly don’t want to end there, because we would like to be able to expand this new model to a broader set of patients as well.
The Pulse: It continues to be a challenge for primary care physicians to remain independent due to market consolidation trends, COVID-19 dynamics, etc. How do you support primary care physicians to remain independent and do you see these trends as risks for Pearl Health?
Rabiner: I read this year that the share of primary care doctors who remain independent has dipped below 50% in this past year. Covid-19 exacerbated trends that were already challenging for primary care. We all heard the stories in early 2020 of physicians going bankrupt, closing practices, or laying off staff because their revenue stream was interrupted by not being able to see patients. In a capitation model, those physicians would have been paid a stable amount each month for each beneficiary aligned to them. They wouldn’t have been waiting for a rule to change to see patients via telehealth and bill for it. Stabilizing the core revenue stream for a primary care practice can really help them, in light of Covid-19 for example, stay independent.
Another perspective is that independent primary care practices often don’t have the resources to easily adapt to evolving business models and regulatory landscapes like a large organization might. We want to serve as an advisor and partner to navigate and be successful in the world of risk-shared and value-based care. It’s a complicated evolution, and Pearl can be a trusted partner and help them remain independent and operate well in this new world.
The Pulse: How do you see technology playing a role in Pearl’s mission?
Rabiner: Tying back to our mission to democratize access to value in healthcare, if we really want to democratize access and open up this world to more providers, we need to make it easier for providers to assess these programs and succeed in taking on the amount of risk that’s right for them. Technology is the key to making these programs more accessible in each stage – the assessment of which program is right for them, and the different insights, actions, and tools they need to be successful once they’ve decided to participate.
Our technology can take on the complexity inherent in these programs, and distill this complexity into streamlined, low friction, delightful experiences for our providers and their patients. Instead of thinking about the providers as a secondary audience for success, we are putting them front and center as we build out our product.
The Pulse: Pearl Health talks about building an “efficient marketplace” – can you share what you mean by this and what success looks like?
Rabiner: There are two different ways we’re thinking about the marketplace. First, we’ve simplified how we talk about reimbursement, but when you dig into how things are calculated in Medicare and how to use the data, it’s really complicated. When we go to PCPs who are contemplating different options — for example, stay in an Accountable Care Organization (ACO), shift to a Direct Contracting Entity (DCE), which DCE, what about this commercial payer — we want to help identify the best option for them. We want to help both physicians and payers find the right matches based on practice patterns, parameters of the program, risk tolerance of the physicians, etc.
Second, there are a number of specialty service companies and start-ups emerging that manage very specific conditions, like renal disease. This is another form of marketplace we envision facilitating. Putting myself in the shoes of an independent primary care physician, I don’t have a data analyst or someone assessing every commercial program, Medicare program, or every great partner who could help my patients. Pearl will have the data to identify which patients have certain conditions, which patients are well managed, and which patients need specialized care. The right intervention might be something a PCP can do on their own, or decide to refer to a partner. We can build a marketplace of condition-specific partners to which our PCPs can refer their patients if that is the right call.
The Pulse: Can you share more about your role as CPO and the team at Pearl Health?
Rabiner: My job as CPO is to create a technology platform to enable everything we’ve talked about today, staying focused on the challenges physician practices are facing and solving those problems through our product. In my role, I work with other company leaders to define how we’re moving forward as a company, and participate in developing our strategy and execution plan. In product management, we translate our company strategy into a product roadmap that drives client value and, ultimately, business value to the company.
I lead four verticals right now. First, the Product Management team that drives our overall product roadmap. Next, the User Experience (UX) team – we want our platform to be delightful to use, so we’ve set a high bar for our UX. Third, we have a Product Partnerships function, which focuses on data acquisition and other partnerships we need to build out the product. Finally, Market Success is our customer-facing group who is out there working every day with our clients. Our team is lean and growing – we just recently reached about 30 people across the company.
The Pulse: As you think about your experience building at early stage companies, what advice would you offer students who are looking to deliver value in healthcare?
Rabiner: Whether it’s product, operations, engineering, customer success – success is really about the ability to take a concept or idea that is great / inspiring and learn how to make it come to life. At athenahealth, I was assigned to a product that had been acquired right before I started, so it was almost like working at a little startup. That was my first role in product management. I’m so grateful that I had that experience – rolling up my sleeves and learning how to really get things done.
In product, you need to be good at both creating strategic vision, and also putting those ideas into action. When you’re great at strategy, you’ll be better at execution because you’ll make different choices if you understand where you’re going and why you’re going there. If you understand what it takes to deliver great execution, you’ll create a better strategy because it will be grounded in what it actually takes to make something come to life.
I would also recommend shadowing healthcare providers or administrators if you haven’t had the opportunity to do that. In the beginning of my career, I worked in billing offices alongside people operating these processes every day. If you can really understand what the day-to-day of your clients or users is like, you’ll take that experience and build it into what you’re doing. Any time I’ve shadowed a provider, talked with a provider, or even met with an unhappy client, I’ve come away really inspired and brought that to bear in my work. It also keeps you humble. You can talk about everything that is broken in healthcare and how it should work in a classroom or a board room, but it’s humbling to go see how it does work and understand that the delta is pretty big. You need to understand how to meet providers where they are and help them move forward.
The last thing I’ll say is that Pearl is always hiring if you are really passionate about improving healthcare!
Interviewed by Lauren Gardanier, December 2021.